Breast Ultrasound
What is a breast ultrasound? Breast ultrasound is the examination of the breast tissue using an ultrasound scan. Ultrasound uses…
Read more
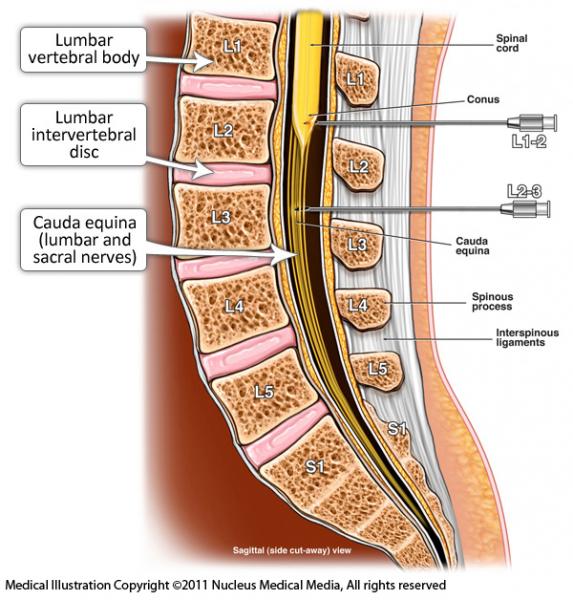
The spine is made up of bones called vertebrae. At the front of the spine is solid bone, and at the back there is a bony canal, or channel called the spinal canal.
The spinal canal contains a fluid-filled tube extending from the base of the skull to the tailbone. This is called the thecal sac and the fluid is called cerebrospinal fluid (CSF). The spinal cord and nerves to the body are contained in this CSF filled sac. A puncture is made into the thecal sac with a spinal needle and a water-soluble contrast medium (sometimes referred to as a contrast agent or X-ray ‘dye’) is injected into the sac. Contrast medium is used in medical X-ray imaging to show the inside of the body on an image or picture. This procedure is referred to as myelogram. A puncture of the thecal sac is called a lumbar puncture.
Myelograms are now carried out much less often than they were 20 years ago. They are used to examine the spinal cord and nerves that come out of the spinal cord to look at spinal and disc problems. Advances in technology allow radiologists (specialist doctors) to see the nerves and cord directly, using magnetic resonance imaging (MRI) instead of X-rays. In some special circumstances, a myelogram is still used to investigate problems involving the spinal cord and spinal nerves. These include:
You should wear comfortable clothes that are easy to remove and leave jewellery at home Please note that some of the disinfectant agents used during these procedures may stain light-coloured clothing. When you make your appointment for the myelogram, you need to let the radiology clinic or department know if you are taking any blood thinning medication, such as warfarin, clopidogrel, dabigatran, prasugrel, dipyridamole or asasantin (for more information about these medications, go to NPS: www.nps.org.au/medicines).
Blood thinning medications may need to be stopped for a period of days, or your normal dose reduced, before this procedure is carried out. It is very important that you do not stop any of these medications or change the dose without consulting both the radiology clinic or department and your own doctor. They will give you specific instructions about when to stop and restart the medication. These drugs are usually prescribed to prevent stroke or heart attack, so it is very important that you do not stop taking them without being instructed to do so by your doctor or the radiology practice, or both. Aspirin is usually not stopped.
A blood test may be required to check your blood clotting on the day of the procedure.
Continue with pain medication and other medications as usual.
You will be asked to change into a hospital gown in a changing room, and someone will look after your clothes and valuables during the procedure. You will be taken into the room where the procedure is carried out, called a fluoroscopy suite.
You will be asked to lie on your stomach on the fluoroscopy table, which is covered with a thin foam mattress and you may have a pillow under your stomach. The table has an X-ray machine under it and a screen over the top of it, as well as a television screen where images or pictures of the inside the body can be viewed directly by the radiologist carrying out the procedure (while the procedure is being carried out).
Your lower back will be cleaned with antiseptic fluid, which is usually very cold, and draped with sterile towels. Local anaesthetic is injected through a small needle in the middle of your lower back. This will numb the skin and deeper tissues. This is uncomfortable for a few seconds, producing a pin prick and a stinging sensation. You will be awake and only the area where the myelogram is being carried out will be numb.
When the skin and muscles are numb, a thin spinal needle is guided into the bony spinal canal and it then punctures the thecal sac. Spinal fluid comes out of the needle and shows the doctor that the needle is in the thecal sac. The X-ray machine will be used to guide the radiologist locating the place for the injection and passing the needle into this spot. Iodine containing contrast medium, usually approximately 10 mL, is then injected into the fluid around the spinal cord. The table may be tipped a little so that your feet are a bit lower than your head when the contrast is injected to make the contrast run downwards into the lower back if you have lower back problems. The needle used to inject the contrast is then removed and a number of X-rays are taken. You will be asked to roll slightly onto each side, onto your back, and to stand while these pictures are taken. The table may also be tipped so that your head is lower than your feet in order to make the contrast that has been injected run upwards into your neck or into your head. This is commonly done if you have neck problems or a question of leakage of CSF into your nose.
You may then be transferred to a room where there is a computed tomography (CT) scanner and asked to lie on the table, either on your back or stomach, and further pictures of the spine will be taken using the CT scanner.
On rare occasions, the spinal needle puncture will be carried out on your neck if lumbar (lower back) puncture is not possible or prevented by skin infection or dressings on the skin of your lower back.
Headache is the major after effect. It can be quite severe, but fortunately is relatively short-term for most people. It is minimised by bed rest for 24 hours and having plenty of fluids to drink.
Any back pain you already have may be made worse by the extra pressure of the injected fluid. The fluid is absorbed by the body over the few hours after the myelogram, and the extra pain decreases when this happens.
Sometimes it can be hard to get the needle into the fluid sac and the myelogram cannot be done. This is often the case in people with severe narrowing in the bony spinal canal as a result of arthritis and disc disease.
The time varies depending on the area to be examined. If the procedure is being carried out on your lower back (the most common area), it will take approximately 30 minutes. If the procedure is being carried out on your lower back and neck, it will take approximately 45 minutes. The CT scan is usually carried out approximately 15 minutes after the myelogram and X-ray images are taken, and takes approximately another 15 minutes.
Myelography is a very safe procedure with minimal possible risks.
Myelography can be very helpful for diagnosis and management of acute or chronic spinal problems, and diagnosis of CSF leakage.
The myelogram will be carried out by a radiologist, trained in carrying out radiology procedures and interpreting X-ray images. The radiologist will be assisted by the radiographer, who is the technician who operates the X-ray machine while the procedure is carried out and the CT scan afterwards.
A myelogram is usually carried out in a private radiology practice or hospital radiology department equipped with X-ray screening where there is fluoroscopy available and a CT scanner.
Fluoroscopy equipment is where the X-ray images can be watched on a TV screen as the procedure is being carried out.
The time that it takes your doctor to receive a written report on the procedure you have had will vary, depending on:
It is important that you discuss the results with the doctor who referred you, either in person or on the telephone, so that they can explain what the results mean for you.
American patient information site developed by the American College of Radiologists (ACR) and the Radiological Society of North America (RSNA).
www.radiologyinfo.org/en/info.cfm?pg=myelography
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.