Biliary Drainage
What is a biliary drainage? Biliary drainage is the insertion of a tube into the bile duct. This is most…
Read more
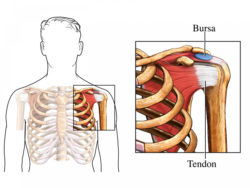
Figure 1
A bursa is a soft tissue space between two structures, such as bone, muscle, tendon and skin, which allows the structures to slide over one another. Soft tissue, such as muscle, fat and skin, connects and surrounds the bones and internal organs of the body.
The most commonly injected bursas are around the shoulder (subacromial bursa) and hip (trochanteric (submaximus) bursa), but a bursal injection might also be helpful in many other areas of the body. These include the elbow (olecranon bursa) and the knee (prepatellar bursa).
Ultrasound is most often used to guide the placement of a needle directly into the bursa, with an injection of corticosteroid (‘cortisone’ or ‘steroid’) and local anaesthetic medication.
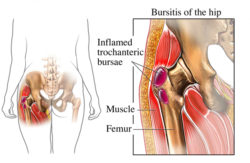
Figure 2
Your doctor would refer you for this procedure if bursitis was thought to be the cause of your symptoms. Bursitis (inflammation of a bursa) is a common cause of soft tissue pain. Movement of the affected area might be painful and you might also have reduced movement. Injection of a small dose of corticosteroid and local anaesthetic into the bursa might relieve these symptoms by reducing inflammation in or around the bursa.
Bursitis in the shoulder might also be felt as pain in the upper arm. Bursitis around the hip is usually over the lateral aspect (outside) of the hip, where the gluteal muscles are located. These muscles lie within your buttock, and extend to the top and outside of the upper femur (leg bone). You are more likely to feel focal tenderness (pain when pressing) over the bone on the outside of the hip, and pain can sometimes go down the outside of your thigh. Both shoulder and lateral hip bursitis can give you pain at night and disturb your sleep.
No specific preparation is needed. You should take any previous X-rays, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) scans to the appointment.
When you make your appointment for the bursal injection, you need to let the radiology facility know if you are taking any blood thinning medication, particularly warfarin.
Blood thinning medications might need to be stopped for a period of days, or your normal dose reduced, before this procedure is carried out. The radiology facility or your own doctor will give you specific instructions about whether you need to stop or reduce the medication and when to restart the medication. These medications are usually prescribed to prevent stroke or heart attack, so it is very important that you do not stop taking them without being instructed to do so by your doctor or the radiology practice, or both.
A blood test might be required to check your blood clotting on the day of the procedure.
Continue with pain medication and other medications as usual.
You will most likely be asked to change into a gown. This will depend on the area that is being injected. You will lie on a scanning bed or sit in a chair in a comfortable position, usually in an ultrasound room. A radiologist (specialist doctor) and/or the sonographer (ultrasound technician) will explain the procedure to you. You will be able to ask any questions.
The area to be injected is imaged to locate the bursa. Sometimes a mark is placed on the skin by the doctor to help guide the needle into the correct place. The skin is then cleaned with antiseptic liquid. A fine needle is passed directly into the bursa using ultrasound images to guide the placement of the needle. Occasionally, the needle is inserted at the point of maximum tenderness for a lateral hip injection, without using ultrasound guidance. A small amount of corticosteroid and local anaesthetic (usually just a few millilitres) is injected and the needle is removed. The needle is generally in and out again within a minute. Most people are surprised by how quick the procedure is.
The doctor will then give you instructions for after the injection. This will generally include completely resting the limb or the part of the body injected for 6 hours, and then limiting its use for between 1 and 3 days, sometimes longer.
As with any injection, there is sometimes a dull ache for a few hours after the procedure. There might be an area of numbness around the injection site, for 1 or 2 hours, due to the local anaesthetic. Some bruising and a few spots of blood at the site of the injection might occur.
The corticosteroid does not usually start working for 24 hours, and sometimes this takes up to 3 days. During this time, the normal symptoms might continue or occasionally worsen. If symptoms are much worse, it generally indicates a reaction to part of the injected medication or to the injection itself. If you find this worrying or distressing, you should see your own doctor or contact the radiology facility where the procedure was carried out.
Sometimes people can experience general reactions, such as flushing and redness of the body and face, related to the absorption of the corticosteroid into the body. These occur over the first few days. In diabetics, the absorption of the corticosteroid can increase the blood sugar levels (BSL) for a few days and the BSL should generally be checked several hours after the procedure.
The procedure itself rarely takes more than 5 minutes, and with the preparation (scanning, marking, explaining the procedure etc.) it will take approximately 15 minutes. If your own doctor has requested an ultrasound to assess the area as well as an injection, this can take up to 30 minutes.
This is a very safe procedure with few significant risks. Few people complain of side-effects, but occasionally problems are experienced.
The aim of a bursal injection is primarily to reduce any inflammation in or around the bursa by injecting a small dose of corticosteroid and local anaesthetic. This should result in pain relief and swelling reduction.
Sometimes the injection is carried out to assess if the bursa is the cause of your pain. A good response to the injection confirms that the source of pain is the bursa that was injected. If there is no improvement in your pain, it is unlikely to be arising from the bursa or the adjacent structures. This can be helpful information for your own doctor, as it means that other causes need to be investigated.
The bursal injection is carried out by a radiologist (specialist doctor). A sonographer (ultrasound technician) will in general carry out the ultrasound and assist the doctor. The doctor will provide a written report, which is sent to your own doctor, detailing the results of the scan and the procedure.
A bursal injection is usually carried out in either a hospital imaging department or a private radiology or nuclear medicine practice.
The time that it takes your doctor to receive a written report on the test or procedure you have had will vary, depending on:
Please feel free to ask the private practice, clinic or hospital where you are having your test or procedure when your doctor is likely to have the written report
It is important that you discuss the results with the doctor who referred you, either in person or on the telephone, so that they can explain what the results mean for you.
The relief of symptoms from the bursal injection might last a few weeks to several months. It is therefore only part of an overall plan for managing your symptoms. You would most likely have been advised to rest the affected area and also change the way you carry out some of your activities. You might have been taking anti-inflammatory tablets and having physical therapy to help the symptoms settle.
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.