Radiation Risk of Medical Imaging for Adults and Children
What is radiation – am I exposed to background radiation each day even if I do not have an X-ray…
Read more
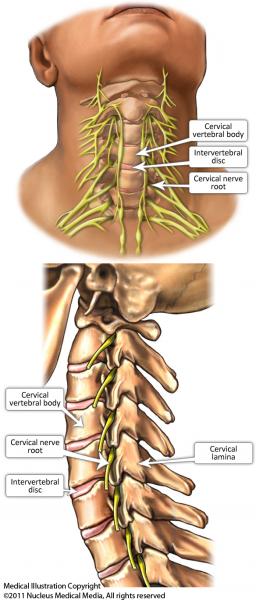
The spine is made up of bones called vertebrae. Between each vertebra is a ‘disc’ that allows the spine to be flexible. The nerves that provide sensation and power to the upper limbs are called
cervical nerves. They exit the spine through openings between two adjacent vertebrae called the intervertebral foramina. There are eight cervical nerves on each side of the neck. The nerve roots are surrounded by fat.
A cervical nerve root sleeve injection is where anti-inflammatory medication called corticosteroid (or ‘steroid’) and a local anaesthetic are injected into the fat surrounding the nerve root. Corticosteroid medication decreases inflammation in the nerve root and will often reduce pain caused by nerve root inflammation, irritation caused by arthritis or conditions such as a prolapsed disc (where the disc bulges) in your neck.
Irritation, compression and inflammation of the nerve caused by a prolapsed disc or a bony spur from arthritis in the neck can cause arm and neck pain. This is more common in older people, but can occur in anyone who has arthritis in the neck. It can also occur after a neck injury.
Your doctor may refer you for relief of this pain in the following situations:
You may have a light meal up to 2–3 hours before the procedure.
You should wear comfortable clothes that are easy to remove and leave jewellery at home, especially necklaces. Please note that some of the disinfectant agents used during these procedures may stain light-coloured clothing.
When you make your appointment for the cervical nerve root sleeve injection, you need to let the radiology clinic or department know if you are taking any blood thinning medication, such as warfarin, clopidogrel, dabigatran, prasugrel, dipyridamole or asasantin (for more information about these medications, go to NPS: www.nps.org.au/medicines).
Blood thinning medications may need to be stopped for a period of days, or your normal dose reduced, before this procedure is carried out. It is very important that you do not stop any of these medications or change the dose without consulting both the radiology clinic or department and your own doctor. They will give you specific instructions about when to stop and restart the medication. These drugs are usually prescribed to prevent stroke or heart attack, so it is very important that you do not stop taking them without being instructed to do so by your doctor or the radiology practice, or both. Aspirin is usually not stopped.
A blood test may be required to check your blood clotting on the day of the procedure.
Continue with pain medication and other medications as usual.
You may be monitored for 2–3 hours after the procedure in the hospital, so please allow for this. You will need to arrange for someone to take you home, as it is not advisable to drive immediately after the procedure, because you may have numbness, weakness or other temporary side-effects after the procedure.
You will be asked to change into a hospital gown in a changing room, and someone will look after your clothes and valuables during the procedure.
You will be taken into the room where the procedure is carried out, either a computed tomography (CT) scanner room or an angiography suite. You will be asked to lie on your back on the table, which is covered with a thin foam mattress. The table has an X-ray machine under it and a screen over the top of it. There is a television screen where images or pictures of the body can be viewed directly by the radiologist (specialist doctor) carrying out the procedure. With a CT guided procedure, the table moves into the CT tunnel and cross-sectional images of the spine are taken.
The nerve root to be injected is located and an ink mark is placed on the skin to show where the needle will be inserted.
The skin is cleaned with an antiseptic, which is usually very cold. The area is then covered with a sterile drape. The skin and deeper tissues are then injected with local anaesthetic. This produces a pin prick and a stinging sensation that is uncomfortable for a few seconds. You will be awake and only the area where the nerve root sleeve injection is being carried out will be numb.
When the skin and muscles are numb, a thin spinal needle is then guided into the intervertebral foramen where the nerve is located. The CT scanner or an X-ray machine will be used to guide this and may be quite close to your face while the radiologist is locating the place for the injection and placing the needle into this spot.
When the needle is in the correct location, contrast medium (or dye) is injected to ensure that the needle is in the correct space and not in a blood vessel. The contrast contains iodine that makes it visible using an X-ray machine or CT scanner (See Iodine-containing contrast medium (ICCM)).
A combination of a long-acting local anaesthetic and a water-soluble corticosteroid is then injected into the tissues surrounding the nerve root. The placement of the needle and injection of contrast into the foramen may produce some discomfort if the foramen is very tight from disc problems or if there is a bony spur compressing the nerve root. The long-acting local anaesthetic very rapidly numbs the nerve. The area of the limb supplied by the nerve being treated goes numb and the arm, shoulder or hand may feel ‘dead’ for a while. This can be worrying when it happens, but you should be aware that the feeling and movement will recover soon.
If any of the following develop seek immediate medical attention:
The actual procedure itself takes approximately 15 minutes. You may be monitored for 2–3 hours after the procedure, so please allow for this. Monitoring occurs after the procedure to make sure any numbness, weakness or other temporary side-effects of the procedure have worn off before you go home. You will also have your blood pressure and breathing monitored after the procedure.
There are minor, moderately severe, and serious (but rare) risks associated with this procedure. In one group of over 4612 patients undergoing this procedure1, there were no major complications and approximately 30 minor complications that resolved without the need for any further intervention.
The minor complications that can occur are:
The moderately severe complications are very uncommon, but if you have them you should tell the staff at the hospital clinic or department where the procedure is carried out. Many of these complications happen at the time of or very soon after the procedure while you are still at the hospital, and you should tell the staff who are looking after you if you notice any of these.
Serious and permanent, but very rare, complications of this procedure include stroke, spinal cord injury leading to partial paralysis and nerve root injury, these lead to permanent problems with movement and feeling in your arms.
It is hard to be certain about exactly how rare the risk is, because what we know about these complications comes from multiple small studies rather than one large study. Fewer than 1 in 1000 people could expect to experience any of these serious complications if the procedure is carried out by an experienced radiologist. It is thought that these problems generally occur because the corticosteroid medication enters a blood vessel supplying the spinal cord or brain. Having this procedure carried out using a CT scanner or high resolution fluoroscopy equipment, rather than a standard fluoroscopy to guide the placement of the needle and avoid the blood vessels, is thought to make this procedure safer and to reduce the risk of this complication. The use of water-soluble corticosteroids further reduces the risk of complication. These complications, if they occur, happen within minutes of the procedure, so you will still be in the hospital or practice should any of these rare problems occur.
Direct injection of the nerve root may damage the nerve permanently.
Accurate needle placement, high-resolution image guidance and skilled specialist doctors are essential to avoid the major complications that arise as a result of poor quality imaging. It is essential that a water-soluble corticosteroid is used.
The benefits of this procedure are relief of arm and neck pain, and avoidance of or delay in surgery. Pain relief may last days to months. The procedure can be repeated every 2–4 months, as long as no weakness develops in your arms as a result of the injection.
Cervical nerve root sleeve injections are usually carried out by radiologists (specialist doctors) and sometimes by pain-management specialists. The doctor carrying out the procedure needs to be appropriately trained in carrying out this procedure, and recognising and managing any minor and severe complications that may occur.
The procedure must be carried out in or close to a hospital setting with access to anaesthesiology and an intensive care unit (ICU). It is best carried out with either X-ray guidance from CT or high-resolution fluoroscopy equipment that is generally found in an angiography suite of a hospital. Standard fluoroscopy equipment may not be sufficient to allow this procedure to be carried out safely.
The time it takes your doctor to receive a written report on the test or procedure will vary depending on:
Please feel free to ask the private practice, clinic, or hospital when the written report will be provided to your doctor.
It is important that you discuss the results with your doctor, either in person or on the telephone, so that they can explain what the results mean for you.
This procedure is safe when carried out by an experienced doctor using high-resolution equipment. The rarer complications are potentially very serious. Because most people who choose to have this procedure have pain, but not a life threatening condition, these very small but serious risks need to be considered, as do the risks of alternative treatments, such as surgery.
No. The most uncomfortable part of the procedure is the initial injection of local anaesthetic. After this, the rest of the procedure is usually not especially painful.
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.