Nuclear Medicine
What is nuclear medicine? Nuclear medicine is a medical speciality that involves giving a patient a small amount of radioactive…
Read more
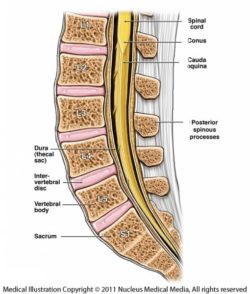
Anatomy of the lumbar spine
The spine is made up of bones called vertebrae. Between each vertebra is a ‘disc’ that allows the spine to be flexible. The epidural space separates the bony spinal canal (the space in the vertebrae through which the fluid filled sac containing the spinal cord passes) from the fluid-filled tube or sac. The nerves to the various parts of the body travel through this space to leave the spinal canal.
An image guided lumbar epidural corticosteroid injection is the accurate placement of a very thin needle, at a given level in this space, under guidance with computed tomography (CT) or X-ray images or pictures to inject corticosteroid (or ‘steroid’) and usually a long-acting local anaesthetic.
The most common reason for your doctor to recommend this procedure is severe or prolonged (chronic) back pain that may or may not go down into your leg or buttock on one or both sides. This procedure is most suitable for people whose back pain is a result of disc or facet joint problems related to ageing and arthritis. It is not recommended for back pain as a result of other causes, such as cancer in the spine or infection. For this reason, it is usual that you will have a CT or magnetic resonance imaging (MRI) scan of the spine to ensure that there is no cause other than age-related changes in the discs and facet joints to explain your back pain.
Epidural corticosteroid injection can sometimes be recommended by your surgeon if you have recurrence of your back pain after surgery. This recommendation will usually come after you have had an MRI scan of the spine to ensure that there is nothing that needs further surgical treatment.
Short-term back pain is best managed by maintaining your normal activities and taking simple analgesics, such as paracetamol, until the pain goes away. Sometimes the pain persists and interferes with normal activities and sleeping. When this happens, other ways of relieving the pain, including epidural corticosteroid and local anaesthetic injection, may be recommended by your doctor.
Because you will be lying on your stomach during the procedure and will be uncomfortable if your stomach is too full, it is advisable to limit food intake to a light meal only, up to 2 hours before the procedure.
It is recommended that you do not drink anything in the 2 hours before the procedure, and you should go to the toilet right before you have the procedure. This is because the local anaesthetic used for this procedure can mean you will not feel your bladder filling as you normally do. This will wear off within an hour or two.
You should wear comfortable clothes that are easy to remove and leave jewellery at home. Please note that some of the disinfectant agents used during these procedures may stain light-coloured clothing. When you make your appointment for the image guided lumbar epidural injection, you need to let the radiology clinic or department know if you are taking any blood thinning medication, such as warfarin, clopidogrel, dabigatran, prasugrel, dipyridamole or asasantin.
(For more information about these medications, go to NPS: www.nps.org.au/medicines).
Blood thinning medications may need to be stopped for a period of days, or your normal dose reduced, before this procedure is carried out. It is very important that you do not stop any of these medications or change the dose without consulting both the radiology clinic or department and your own doctor. They will give you specific instructions about when to stop and restart the medication. These drugs are usually prescribed to prevent stroke or heart attack, so it is very important that you do not stop taking them without being instructed to do so by your doctor or the radiology practice, or both. Aspirin is usually not stopped.
A blood test may be required to check your blood clotting on the day of the procedure.
Continue with pain medication and other medications as usual.
If you have problems lying on your stomach, please advise the practice or hospital when you make your appointment, as this can make the procedure difficult and the radiologist (specialist doctor) carrying out the procedure needs to be made aware of this.
You may be monitored by nursing staff while you lie in a bed in the observation ward for approximately 2 hours before you are allowed to leave.
You will need to have someone take you home, because you are not allowed to drive immediately after the procedure.
You will be asked to change into a hospital gown and leave your belongings in a locker.
You will then be asked to lie on a table on your stomach and this table will either be in the CT scanning room or in a fluoroscopy suite. In both cases, there is equipment over or around the table that allows the radiologist to use X-rays to guide the needle placement. The table will have a thin foam mattress on it and you will have a pillow for your head.
A metal marker will be taped on the skin of your lower back and images or pictures on the fluoroscopy equipment or the CT scanner will be used to adjust the position of this marker so that it is at the correct level for the injection. The skin will be marked with a pen or felt marker to indicate where the needle will enter the skin and the metal marker will then be taken away.
The skin is cleaned with an antiseptic and a drape may be placed on your back. A local anaesthetic injection is used to numb the skin and deeper tissues. This is uncomfortable for a few seconds, producing a pin prick and a stinging sensation. You will be awake and only the area where the lumbar epidural injection is being carried out will be numb.
When the skin and muscles are numb, a thin spinal needle is then guided into the spinal canal and into the epidural space. The placement of the needle in the epidural space is checked by the radiologist by injecting contrast medium (X-ray dye) or air. Contrast medium enables the CT to show the area inside the body where the procedure is being carried out more clearly on the images.
Once it is confirmed that the needle is in the correct position, a mixture of corticosteroid and (in some radiology practices/hospitals) a long acting anaesthetic is/are then injected. The pressure of the injection may momentarily increase the pain, but this is generally quickly relieved as the local anaesthetic takes effect.
Depending on the spread of the local anaesthetic, you may feel total numbness of both legs or one leg for up to 2 or more hours.
Your blood pressure may drop temporarily, as a result of the local anaesthetic, so you will be asked to lie in bed flat on your back, stomach or side, because sitting up could make you feel dizzy. Your lower body and legs may feel ‘flushed’ for a short time.
You may not notice that your bladder is full and may not have the usual control over your bladder in the first couple of hours after the procedure. If your bladder is full, this can sometimes lead to leakage of urine (urinary incontinence) and this is the reason for suggesting that you empty your bladder right before the procedure and not drink anything for a couple of hours before the procedure.
The procedure takes no more than 15 to 20 minutes under CT guidance. It may take longer if X-ray is used. The time taken for full recovery, leg function, bladder function and blood pressure normalisation is approximately 30 minutes to an hour. Some patients require upwards of 2 hours. With preparation time, you should allow 4 hours between entering the radiology practice or hospital and leaving again. You will not be allowed to leave until your legs and bladder function are normal, your blood pressure is normal, and you are able to sit up and walk normally without feeling dizzy.
Image guided injections are accurate and minimise the risks of complications. Very small needles can be used under CT guidance. Relief of back pain and avoidance of, or delay in surgery are the major benefits. The pain relief is often not permanent, but fortunately the injections can be repeated if and when the pain comes back. The generally accepted practice is to limit this to no more than three to four injections per year to minimise the complications of the corticosteroids.
There is rapid pain relief if local anaesthetic is used and this may last 2–4 hours, but the pain may then return. The steroid takes approximately 48 hours to have effect. In some patients, breaking the pain cycle with the steroid injection results in pain relief, which is maintained for several weeks to months.
A radiologist or pain specialist (often an anaesthetist with a special interest in pain management) with appropriate training, using CT guidance or X-ray guidance.
Image guided procedures have been shown to be safer than non-image guided procedures.
An image guided lumbar epidural injection is carried out in a radiology department or practice, an operating theatre suite with suitable image guidance CT or X-ray equipment, or an angiography suite (again, within a hospital or radiology practice).
The time it takes your doctor to receive a written report on the procedure will vary depending on:
Please feel free to ask the private practice, clinic, or hospital when the written report will be provided to your doctor.
It is important that you discuss the results with your doctor, either in person or on the telephone, so that they can explain what the results mean for you.
No. The most uncomfortable part of the procedure is the initial injection of local anaesthetic. After this, the rest of the procedure is usually not especially painful.
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.