Chaperone
Patients can find examinations, investigations or taking images (or pictures) of an intimate nature, i.e. involving the breasts, genitalia or…
Read more
A magnetic resonance imaging (MRI) scanner uses strong magnetic fields to create an image (or picture) of the prostate and surrounding tissues.
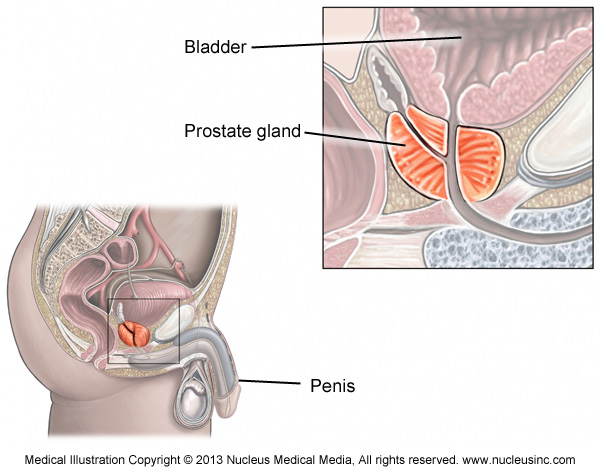
The prostate gland is a small soft structure about the size and shape of a walnut, which lies deep in the pelvis between the bladder and the penis, and in front of the rectum (back passage).
Its function is to help liquefy semen (produced from the male sexual organs to fertilise the female egg).
Your doctor might request an MRI of the prostate gland for a number of reasons:
MRI is generally requested because it provides more detailed images of the prostate gland than other radiological tests, such as computed tomography (CT) or ultrasound.
There is no special preparation for the scan. You should continue to take any regular medications, and generally eat and drink as normal. Some radiology practices might ask you to have a liquid diet for 24 hours before the MRI scan.
Before the examination begins, you will be asked a series of questions about whether you have any metal implants, such as artificial joints, or electronic devices, such as pacemakers, inside you.
Some of these can cause you harm or be damaged if they are put into the strong magnetic field of the MRI machine. If you have a heart pacemaker, please tell the radiology practice where you are having the MRI scan as soon as possible before the appointment.
You should take any documents or information you have about the metal implants inside you, to assist in deciding if the scan can be carried out safely.
Some metal bands and loops of wire (e.g. some necklaces) can become quite hot if put into the scanner, so you will be asked to remove any such metal before entering the scan room.
If you have previously become claustrophobic during an MRI scan or think the confined space in the MRI machine might cause you to become claustrophobic, please discuss this with your own doctor or when you make the scan appointment. You might require sedation, and it is best to have a friend or relative bring you to your scan appointment and drive you home.
You will be asked to change into a hospital gown and lie on a table attached to the MRI machine. A small needle will be inserted into a vein in your arm or hand; this will be used to give the following medications:
Some radiology practices use an endorectal (inside your rectum) coil as part of the scan. An endorectal coil is a latex (rubber) balloon with a central tube that contains the coils. It helps to provide high-quality images of the prostate and surrounding area. It is inserted into the rectum and inflated before the scan. It stays in during the scan and is removed when the scan is finished.
Some radiology practices also give an enema before the procedure. An enema is a liquid that is squirted into the rectum via the anus (opening of the back passage to the outside) and helps to clear the bowel. Again, this is to provide as high-quality images as possible.
As the MRI machine produces loud knocking noises, you will either be given earplugs or headphones to lessen the noise of the machine during the scan. If the MRI machine has headphones, you can take your favourite CD or an MP3 player to listen to while you are having the scan.
The table on which you are lying will then be moved into the MRI machine. The MRI machine is a large box with a central tunnel. Depending on the type of MRI machine being used, your feet might go in first with your head and neck outside the scanner or your feet might be outside.
The scan takes approximately 30 minutes (several individual scans of a few minutes each). You are required to lie as still as possible during each scan. If you think that lying still for this amount of time might be a problem for you, please discuss this when you make your appointment for the scan. You do not have to hold your breath or move into any special positions during the scan.
There are no after effects of the scan itself.
It is rare, but the Buscopan injection can cause a dry mouth and mild blurring of the vision. These should last no more than 1 hour. If you experience blurred vision, you should not drive, but as this is a rare and short-lived after effect, it is not necessary to plan to have someone drive you to and from your scan.
If you are given a sedative, you might feel drowsy for some time afterwards and will not be able to drive home. You will need someone else to drive you home.
Occasionally, there might be a few spots of blood after removal of the endorectal coil, especially if there has been a recent prostate biopsy. Please contact the MRI facility if this occurs.
A prostate MRI generally takes approximately 30–45 minutes.
A very small number of people have an allergic reaction to the gadolinium contrast medium. Most reactions are mild, such as a rash or hives (itchy spots).
If you have very poor kidney function, you will not be given contrast medium, as there is a small risk of nephrogenic systemic fibrosis – see Contrast Medium: using gadolinium or iodine in patients with kidney problems.
If an endorectal coil is used for the scan, there is also a very small risk of damage to the rectum from the balloon. If you have any concerns, please contact the MRI facility.
The MRI scan can help find a cancer of the prostate gland, especially if you have elevated or rising PSA.
If a cancer has already been found, the MRI images can show whether it has spread outside the prostate gland or not. This can have a very important impact on whether or not you have treatment, and if so, which type of treatment you receive.
A radiographer (also called a medical imaging technologist) prepares you for the scan and operates the machine while the scan is being carried out.
The images that the radiographer produces are interpreted (or ‘read’) by a radiologist (specialist doctor).
A prostate MRI scan can be carried out at a hospital radiology department or private radiology practice.
The time that it takes your doctor to receive a written report on the test or procedure you have had will vary, depending on:
Please feel free to ask the private practice, clinic or hospital where you are having your test or procedure when your doctor is likely to have the written report.
It is important that you discuss the results with the doctor who referred you, either in person or on the telephone, so that they can explain what the results mean for you.
American College of Radiology: www.radiologyinfo.org/en/info.cfm?pg=mr_prostate
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.