SAH Vasospasm Endovascular Treatment
What are the prerequisites for having a SAH Vasospasm Endovascular Treatment done? Consultation with the treating specialist (neurosurgeon or neurointerventionist)…
Read more
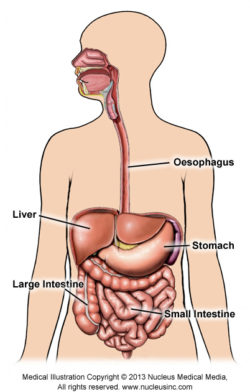
Figure 1: Digestive System
A paediatric barium meal is a study to examine a child’s stomach and small intestine (or bowel).
It is sometimes carried out with a barium ‘swallow’, to show the oesophagus (the tube connecting the mouth to the stomach), or with a barium ‘follow through’, to show the small intestine.
Barium (a chalky substance) is mixed with water and makes a white liquid. When this is swallowed, the oesophagus, stomach and small intestine can be seen on X-ray images or pictures.
Your doctor has referred your child for this procedure to investigate the causes of upper abdominal pain and/or persistent vomiting, particularly if blockage or twisting of the upper intestine is suspected. The paediatric barium meal can show the position and size of the stomach and small intestine, and if there is a blockage.
The most important preparation for your child is to not eat or drink before the study, as any food in the stomach makes a paediatric barium meal difficult to interpret. The length of time your child will need to go without food or drink (called fasting) will depend on their age. Very young children will only be asked to fast for 2 hours, but older children will be asked to fast for up to 4 hours.
This can be difficult for some children and parents. It is often best to have the barium meal appointment early in the day, so your child is awake for as little time as possible without being able to eat or drink.
If your child takes medications with clear liquids, these can be taken with a small amount of water up to 1 hour before the study. If your child needs to take medication with food, then you will need to discuss the timing of the medication and barium meal study with your doctor.
Metal buttons and zips, and some types of material can be seen on X-ray images, making the study more difficult to interpret, so your child will be changed into a hospital gown. It is best if your child wears clothing that is easy to take off and put back on.
If your child is old enough to have some understanding of what is happening, talking about the study with your child before attending the test should help to reduce his/her anxiety. If a parent or carer is anxious, then the child usually notices this and will often also become anxious or frightened. As the parent or carer, we strongly encourage you to find out about the test to reduce any concerns or fears you might have before you attend with your child. You can ring or visit the X-ray facility for more information. You can also read the item ‘Making your Child’s test or procedure less stressful – advice to help you and your family’.
Your child will be asked to lie on his/her side or back on the bed (table) of the X-ray fluoroscopy machine. They will usually be asked to change positions during the study. When the images are taken, your child needs to be still, so that the images are not blurry.
Your child will be given a drink of a liquid called barium. Barium is like a thick, slightly chalky-feeling milkshake with flavourings added to make it easier to drink.
The barium can be seen on images taken with the X-ray fluoroscopy machine. Fluoroscopy shows the inside of the body as it is working, which can be watched like a movie on a screen. Barium makes a shadow by stopping the X-rays, and showing the inside of the stomach and small intestine. Images are taken as the barium moves through the stomach and small intestine.
If your child is unable or unwilling to drink the barium, the barium can be given by bottle, squirted into the mouth with a syringe or injected down a nasogastric tube (a thin tube passed into the stomach through the nose). Older children, who prevent any of these methods from being used, might need to have a different study. Children should not be forcibly held down for an X-ray examination.
If your child is having a follow-through examination, images of the abdomen will be taken over a longer period of time; usually 2–8 hours, but sometimes longer. Images are taken at intervals of between 10 minutes to over an hour, which might be taken in a different X-ray room. Your child might be encouraged to drink more barium or eat food to speed up the passage of the barium through their bowel. In the time between the images, the child might be encouraged to lie on his/her right side or more likely be told to walk around; this can be outside the X-ray department if the child is not unwell.
The barium that is swallowed will pass through the intestines and be seen in your child’s bowel motions (faeces) as a white paste. The barium can cause your child to be a little constipated, so he/she should drink plenty of fluid and increase their fibre intake after the study to reduce the risk of this occurring. One or two extra glasses of water or clear liquid and one or two extra serves of fruit or vegetables will be of benefit.
Your child can return to school, kindergarten or child care after the study, unless there is a medical reason not to do so.
A paediatric barium meal will take approximately 10–20 minutes unless it includes a ‘follow-through’ examination.
A follow-through examination can take several hours (usually 2–8 hours, but sometimes longer), as the barium has to pass all the way through the small intestine.
If your child requires a follow-through examination, you and your child could be at the hospital or radiology practice for some considerable time. Talk to the X-ray staff about how you and your child’s time at the facility will be managed during the study.
The barium meal study might not show an abnormality that is present, and further investigations might be required to confirm a diagnosis. Your referring doctor will discuss the test results with you.
X-rays are invisible and pass through the body without any sensation. X-rays, like many other medical investigations and treatments, are not considered harmful if used appropriately (see Radiation Risk of Medical Imaging for Adults and Children).
A paediatric barium meal easily shows the outline of the stomach, the first part of the small intestine and any abnormal position of the stomach. It does not require your child to be sedated or admitted to hospital and has minimal risks.
It more easily shows the position of the stomach and small intestine than other tests.
The images are usually taken by a radiologist (specialist doctor) who carries out the study with the assistance of a radiographer and often with the assistance of a nurse. The medical staff will ensure the least amount of distress for your child.
Barium meal studies are carried out in a special X-ray fluoroscopy room of a private radiology practice, or in a public or private hospital.
The time that it takes your doctor to receive a written report on the test or procedure your child has had will vary, depending on:
Please feel free to ask the private practice, clinic or hospital where your child is having their test or procedure, when your child’s doctor is likely to have the written report.
It is important that you discuss the results with the doctor who referred your child, either in person or on the telephone, so that they can explain what the results mean for you and your child.
In some instances, the barium meal study will be carried out using a different liquid (water-soluble iodine-based contrast, see Iodine-containing Contrast Media) that also shows up on the X-rays. It can be used if there is no need to look closely at the mucosa (lining) of the stomach or small bowel. This liquid looks like water and will not be seen in the bowel motions.
Page last modified on 29/3/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.